Sports Medicine

WHAT IS SPORTS MEDICINE?
Our world-renowned sports medicine experts are ready to help your injured athlete get back in the game. We have unparalleled experience providing non-operative and arthroscopic care to treat common sport-related injuries including concussions, ligament injuries and cartilage conditions in the knee, ankle, shoulder, elbow and hip in young and growing athletes.
Board-certified pediatricians, pediatric orthopedic surgeons, physical therapists, athletic trainers, psychologists and other sports medicine specialists work side by side with each athlete, their parents and coaches to develop the best game plan for treatment, rehabilitation and safe return to sport.
We enjoy hearing about our current and former patients' success stories. Tell us about your MVP.
Sign up to receive our digital newsletter with tips and insights for parents of young athletes.
OUR SPORTS MEDICINE SERVICES
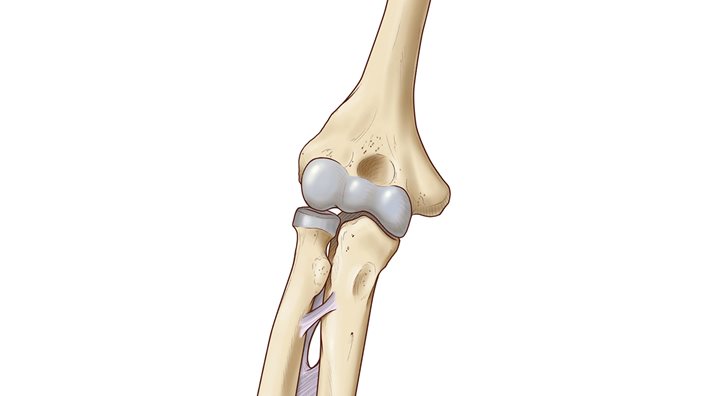
ELBOW
The elbow is a combination hinge-and-pivot joint made up of three bones: the upper arm bone (humerus) and the two bones in the forearm (radius and ulna). The hinge part of the joint lets the arm bend like the hinge of a door; the pivot part lets the lower arm twist and rotate.
Muscles, ligaments and tendons hold the elbow joint together.
Cartilage, or soft tissue, protects the bony surfaces. It’s also found in young bones at areas that are still growing. These growth areas are at risk for injury.
Elbow injuries in young athletes are on the rise, partly due to year-round training and competition. Overuse injuries often occur in throwing sports and gymnastics. Early recognition of signs and symptoms can prevent problems and even career-changing injuries. In youth sports, preventing elbow injuries, particularly those requiring surgery, is a priority.
Learn more about Osteochondritis Dissecans (OCD) in the Elbow.
Pain typically occurs on the inside “bump” of the elbow during or after activity like throwing or pitching. Repeated pulling can tear ligaments and tendons away from the bone. This tearing may pull tiny bone fragments with it in the same way a plant takes soil with it when uprooted. This can disrupt normal bone growth, resulting in deformity and instability with throwing.
SYMPTOMS
- Elbow pain with throwing or after activity
- Pain and tenderness on the inside of the elbow (on the bump)
- Soreness for days to weeks
- Worsening control with throwing
- Inability to throw desired distance
- Difficulty fully straightening or bending the elbow
- Locking of the elbow
TREATMENT
- Rest. Continuing to throw may lead to major complications and jeopardize a child’s ability to remain active in a throwing sport.
- Common recommendations include 2-4 weeks of complete rest.
- Apply ice packs to bring down any swelling.
- Proper stretching and strengthening.
- May require a cast or splint if the pain does not resolve with rest.
- Therapy to focus on flexibility, strength, trunk and scapular stabilization.
- Focused training to improve throwing form is needed.
- Surgery to stabilize the medial epicondyle is rarely necessary, especially in girls over 12 years and boys over 14 years.
With this injury, the athlete will typically hear a pop and will have severe pain, swelling and bruising. The child may or may not have had elbow pain before the injury. With operative or nonoperative treatment, most kids may return to the same level of sports following treatment.
SYMPTOMS
- May hear a pop or giving way
- Immediate pain on inside of the throwing elbow
- Immediate, visible swelling and bruising
- May have pain with wrist movement
- May have numbness or tingling in the ring finger and little finger
- Unable to bend the elbow or pick up heavy objects
TREATMENT
- Ice may be helpful to reduce inflammation in early stages.
- Anti-inflammatory medication may be needed.
- For fractures in good position, a splint is recommended for 2-3 weeks.
- In all cases, aggressive range of motion early in healing stages (within 2-3 weeks) is recommended.
- Therapy to focus on flexibility, strength, trunk and scapular stabilization.
- Strengthening and proper throwing progression 8-12 weeks following injury.
- Focused training to improve throwing form is needed.
SYMPTOMS
- Pain in the back of the elbow during follow-through and when straightening arm
- Pain in the back of the elbow that becomes gradually worse over time
- Inability to completely straighten the arm
- Popping and locking may be present, but is rare
TREATMENT
- Rest. Continuing to throw with this problem may lead to major complications and permanently jeopardize a child’s ability to play.
- Common recommendations include 2-4 weeks of complete rest.
- Ice pack may help reduce inflammation.
- Anti-inflammatory medication may be needed.
- Therapy to focus on flexibility, strength, trunk and scapular stabilization.
- Focused training to improve throwing form is often necessary.
- Surgery is only needed in severe cases.
SYMPTOMS
- Dull achiness on the outside of the elbow
- Pain that worsens with activity and improves with rest
- Pain that gradually worsens over time
- Inability to completely straighten the arm
- Popping and locking
TREATMENT
- Rest. Continuing to throw with this problem may lead to major complications and permanently jeopardize a child’s ability to play.
- Strict throwing restrictions protect the elbow from further injury.
- Immobilization may be necessary in severe cases or if restrictions are ignored.
- If the elbow does not heal or the tissue becomes unstable or loose, surgery may be the best option.
- Therapy to focus on flexibility, strength, trunk and scapular stabilization.
- Resume throwing at a minimum of 6-12 months.
- Focused training to improve throwing form is often necessary.
These injuries rarely occur with a single event or throw. They’re more common in older adolescents, but may occur in younger athletes as well. An MRI with contrast injected in the joint gives the best view of a tear.
The surgical reconstruction of the UCL is named after Tommy John, a baseball player who returned to major league pitching after having this procedure. This surgery doesn’t always lead to improved performance. Though many athletes do return to play after this procedure, preventing the injury is ideal.
SYMPTOMS
- Pain over the inside of the elbow with throwing
- Gradually increasing pain
- May feel unstable or “give way”
- Rarely popping
TREATMENT
- Rest for at least 6-12 weeks. Continuing to throw with this problem may lead to major complications and permanently jeopardize a child’s ability to play.
- Immobilization for 4-6 weeks followed by a hinged elbow brace.
- Anti-inflammatory medication.
- Therapy to focus on flexibility, strength, trunk and scapular stabilization.
- Surgery is typically needed for complete tears or if the elbow is unstable.
- Focused training to improve throwing form is often necessary.
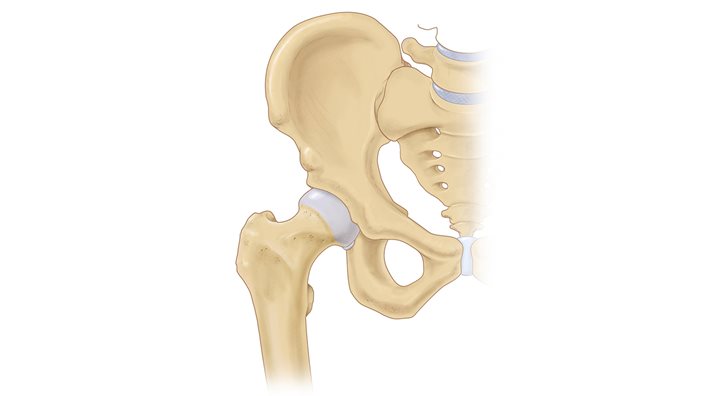
HIP
Conditions we treat:
- Femoral acetabular impingement (FAI)
- Labral tears
- Snapping hip
- Hip and groin strains
- Overuse hip conditions (such as those seen in dancers and gymnasts)
- Pelvic apophysitis
- Pelvic avulsion fractures
ANKLE
Conditions we treat:
- Ankle instability
- Ankle sprain
- Ankle fractures
- Stress fractures of the foot and ankle
- Cartilage conditions such as osteochondritis dissecans (OCD)
- Sever’s disease

CONCUSSION
Concussions continue to get a lot of attention in the media, and for good reason. At Scottish Rite for Children, we continue to study young athletes to learn more about how their brains recover from concussions. We already know that concussion recovery time in children is longer than in adults.
Here are a few additional things our patients have taught us:
- Concussion symptoms are worse and last longer when an athlete continues to play on the same day as their injury
- Girl soccer players are more likely to continue to play on the same day, but boys do too
- Poor sleep is connected to worse concussion symptoms and longer concussion recovery time.
- Anxiety symptoms following a sport-related concussion lead to more time before returning to play.
- In female athletes, delayed presentation to clinic is associated with longer time to clearance to return to play following a sport-related concussion, so it is important to be evaluated soon after the injury.
Learn how to recognize and respond to signs and symptoms of a concussion here or read articles about sport-related concussions on our blog.

Note: There are some signs and symptoms following a head injury that are especially concerning. Seek medical attention immediately at the nearest emergency department if any of the following occur:
- Severe or worsening headache
- Increasing confusion
- Extreme sleepiness or trouble waking up
- Vomiting
- Seizures (convulsions - arms and legs jerk uncontrollably)
- Weak or numb arms or legs
- Slurred speech
- Any other sudden change in thinking or behavior
SIGNS
- Appearing dazed or stunned
- Confusion
- Forgetting plays
- Being unsure of game, score or opponent
- Exhibiting unsteadiness
- Moving clumsily
- Answering questions slowly
- Losing consciousness (getting knocked out)
- Memory loss
- Being more sleepy or tired than usual
- Seeming sad, nervous or anxious
- Being irritable, easily frustrated or upset
- Having problems with academic performance
- Slow to get up after a fall, collision or blow to the head
- Clutching the head after an injury
- Sleep problems
SYMPTOMS
- Headaches
- Concentration or memory problems
- Nausea
- Balance problems or dizziness
- Double or blurred vision
- Feelings of being “in a fog” or slowed down
- Sensitivity to light or noise
- Confusion
- Just “not feeling right” or “feeling down”
A history and physical examination, along with the patient and family’s report of signs and symptoms, along with tests to assess balance, eye movements, memory, reaction time, etc., are utilized to diagnose a concussion and determine the best treatment for the athlete.
To learn more about concussion treatment, view our handout. (English / Spanish).
Return to School
- A school may consider the following accommodations to help a student athlete:
- Reducing homework and class work
- Postponing tests until the student has recovered
- Providing alternative activities for the athlete for taking notes during class, watching videos, being in a loud environment (lunchroom or gymnasium), or participating in physical activity (PE, athletics, recess)
- Allowing a student to take frequent breaks in the nurse’s office or alternating a class with a rest
- Permit the athlete to go to the nurse’s office for worsening of symptoms during classes
Return to Play
Clearance by a health professional is strongly recommended, and, in some cases, required by law, the school or organizational concussion protocol. Returning to play before complete recovery from a concussion puts the athlete at risk for a more serious injury, permanent brain damage and even death, from another injury known as Second Impact Syndrome.
When the athlete has returned to everyday and school-related activities and has no symptoms, make an appointment for an evaluation and sports clearance. For patients with severe or persistent symptoms, a referral to a sports medicine specialist may be helpful.
Concussion protocols are typically designed as a one week return to play progression. This is often misinterpreted as the answer to “how long will a concussion last?” The protocol insists that the five- to seven-day progression begins and only continues when the athlete is symptom free. In college athletes and adults, a week or two is typical. We find that young athletes take longer to recover, even if they are following recommendations. For some, symptoms may last for months. Our goal with treatment and management of concussions is to get an athlete back to school and daily function as efficiently as possible. Then, we begin return to play protocols.
Return to Play Guidelines:
Once the athlete is completely symptom-free, and has been cleared by a health care professional, they may begin a progressive return-to-play protocol. A symptom-free period of 24 hours is required before moving on to the next stage. If symptoms occur during or after activity, the athlete should stop and consult with their health care provider.
Remember, the athlete MUST BE:
- Symptom-free with daily activities and schoolwork (including tests) to begin the protocol.
- Symptom-free during/after exercise to progress to next stage.
Return to Play Progression:
- Begin light aerobic exercise with no resistance – e.g. riding a stationary bike or light jogging for 10-15 minutes.
- Sport-specific activity – e.g. running drill for 20-30 minutes with increased exertion.
- Non-contact training drills with resistance training – e.g. ball handling or passing drills
- Full contact practice (must have physician clearance) – e.g. scrimmage and game-like training drills.
- Competitive game play.
Athletes 5 years of age and older without a recent history of a head injury can take a baseline test, used for future reference (ages 5-12 will be given ImPACTTM Pediatric). For athletes with a recent head injury, we recommend making an appointment with one of our sports medicine physicians before scheduling a baseline test. In the event of a concussion, an athlete can repeat the test and the Credentialed ImPACT™ Consultant (CIC) can then analyze the results. The comparison of the post-injury scores to the baseline test helps the provider develop an individualized plan for the athlete.
Our sports medicine specialists, Shane M. Miller, M.D., and Jane S. Chung, M.D., are Credentialed ImPACT™ Consultants. These physicians and our athletic trainers have undergone specialized ImPACT™ training to administer and interpret this test for use in concussion care management.
PAYMENT
VISIT
A parent may remain in the room with the athlete during the test. If additional family members, particularly young siblings, are present, we request they remain in the waiting area with a parent to allow the athlete to concentrate and for optimal test performance.
RESULTS
FEMALE ATHLETE TRIAD

OSTEOCHONDRITIS DISSECANS
We see OCD most often in patients that are 12-16 years old. Though it can happen to anyone, we see this problem in athletes that perform repetitive motions like running, jumping, pitching or certain motions in gymnastics.
We’re unsure what causes this in some patients. It could be a change in the blood supply to the bone and cartilage. Sometimes an injury causes the changes. This is called an osteochondral fracture or injury.
SYMPTOMS
There may be pain in the joint that gets worse with activity. Or there may be symptoms like popping, clicking or swelling in the joint.
TREATMENT
RETURN TO SPORTS
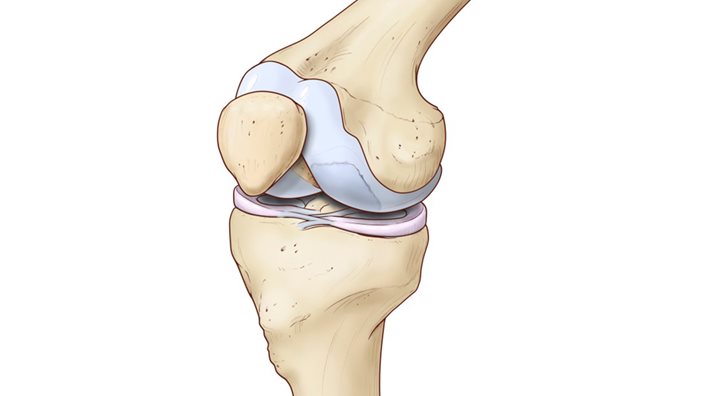
KNEE
Learn more about knee injuries.
.jpg?width=200&height=212&ext=.jpg)
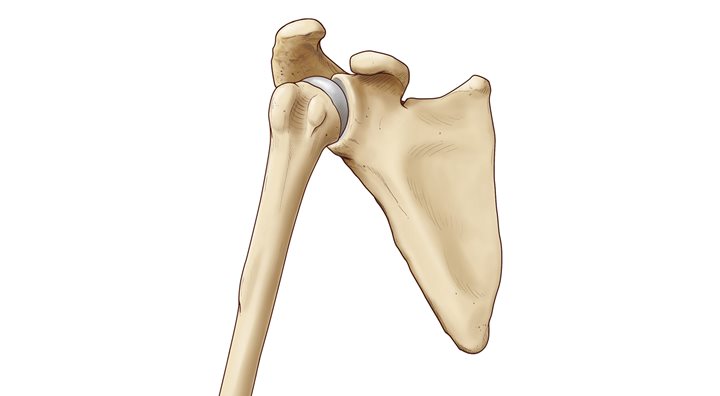
SHOULDER
Learn more about shoulder injuries.

Sports Nutrition
Learn more on the Sports Nutrition page >>