Aug 21, 2019 / Hip Disorders
Recognizing Adolescent Hip Conditions
Key messages from a presentation by staff orthopedist, David A. Podeszwa, M.D., at Coffee, Kids and Sports Medicine. Article originally published in first quarter, 2018 issue of Pediatric Society of Greater Dallas newsletter.
Watch the lecture
Print the PDF
Recognizing Hip Conditions in the Pre-Teen and Teenager
Kids of all ages complain frequently of aches and pains around the hip and it is really easy to brush them
off. I would be lying if I said that I haven’t done it to my own children. For the super-active child/teen who participates in high impact activities year-round, it is easy to explain away complaints of hip pain as simple overuse. The combination of anti-inflammatories, stretching and playing through the pain is a common remedy. At the opposite end of the spectrum is the video gamer or book lover who is more sedentary and less interested in exercise. Their complaints of hip pain are easily attributed to deconditioning and weakness. Becoming more active is the simple remedy. Unfortunately, not all hip pain can be ignored. Missing certain conditions early in their presentation can have significant long-term pain and functional consequences. Below are several important pearls to remember that will help you avoid missing a serious hip condition when evaluating a patient with hip pain.
Watch the lecture
Print the PDF
Recognizing Hip Conditions in the Pre-Teen and Teenager
Kids of all ages complain frequently of aches and pains around the hip and it is really easy to brush them
off. I would be lying if I said that I haven’t done it to my own children. For the super-active child/teen who participates in high impact activities year-round, it is easy to explain away complaints of hip pain as simple overuse. The combination of anti-inflammatories, stretching and playing through the pain is a common remedy. At the opposite end of the spectrum is the video gamer or book lover who is more sedentary and less interested in exercise. Their complaints of hip pain are easily attributed to deconditioning and weakness. Becoming more active is the simple remedy. Unfortunately, not all hip pain can be ignored. Missing certain conditions early in their presentation can have significant long-term pain and functional consequences. Below are several important pearls to remember that will help you avoid missing a serious hip condition when evaluating a patient with hip pain.
- Hip disorders can present with hip or knee pain. Sorting out the etiology and location starts with a good history and physical exam. Is the chief complaint pain, limp, or decreased motion? Some disorders can present without pain and only a limp. Where does it hurt? Hip disorders can present with hip (anterior, lateral, groin), thigh or knee pain. Complaints of constant pain that does not resolve with rest, is worse with weight bearing, limits hip range of motion, and is not improved with anti-inflammatories should be red flags for a significant underlying condition. Physical exam may demonstrate pain with palpation at the anterior superior iliac spine, iliac crest, and or greater trochanter. Pain with range of motion or significant asymmetry in hip range of motion should also be concerning.
- Children and adolescents do not get “groin pulls.” Recurrent limping and/or hip pain (especially groin pain) unresolved with rest is likely to have an underlying etiology. “Groin pull” is an easy answer, but it is never the correct one.
- An adolescent limping with his/her foot turned out and complaining of hip or knee pain has a slipped capital femoral epiphysis (SCFE) until proven otherwise by an AP and frog-lateral of both hips. Range of motion of the hip will likely be painful, especially with internal rotation when the hip is flexed. In severe cases, there will be obligate external rotation (and often abduction) when flexing the hip. In addition, any pre-teen or teen who presents with thigh or knee pain should have their hips examined as well. Referred pain is very common. Examining the hips in the face of knee pain will help prevent you from missing a serious hip condition. Delay in diagnosis is very common and is correlated with a more severe deformity and poorer outcomes.
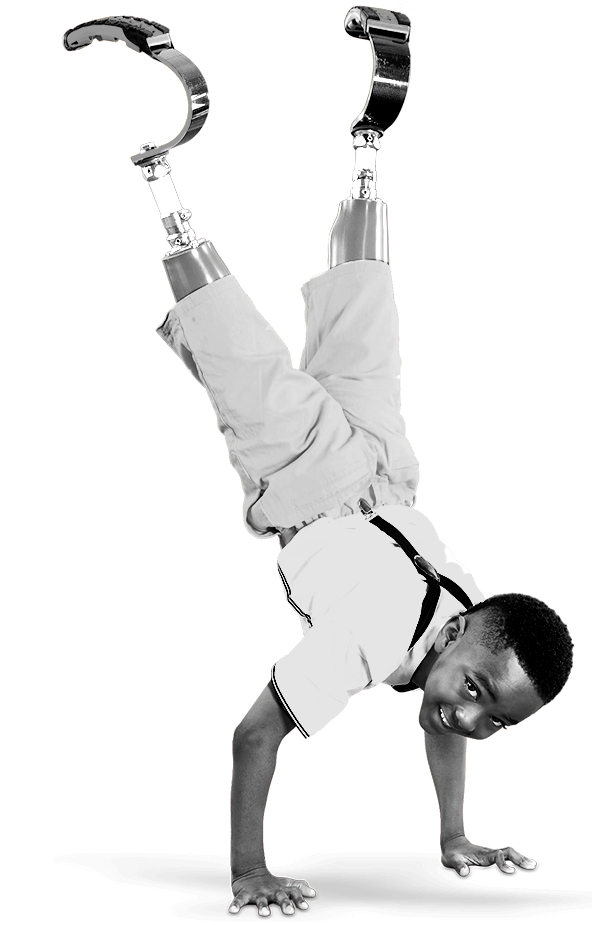
- Hyperactive boys under the age of 10 who present with a limp (without pain or with vague complaints of hip, thigh or knee pain) should have an AP pelvis and frog-lateral of the hip to evaluate for Legg-Calve-Perthes disease. Far more common in boys than girls (4:1), this condition is most common between 4 and 10 years of age. The affected child is usually small and young appearing for his/her age. The child is able to bear weight, the pain or limp is usually worse with increased activity and there will not be any systemic signs or symptoms. Early diagnosis and treatment can make a significant difference in outcome. Once diagnosed, please refer to a pediatric orthopedist.
- Adolescents with hip pain and fever have septic arthritis of the hip until proven otherwise. Transient synovitis most commonly affects children 4-9 years old. Be very skeptical of this diagnosis in any child outside this age range. If the child is younger than four or older than ten years of age with hip pain and fever, think septic arthritis first. The child with transient synovitis may be able to ambulate and may tolerate gentle passive range of motion of the hip. He/she will commonly be afebrile. The CRP is usually <2 mg/dL, ESR usually <40 mm/hr, and WBC usually <12K cells/mL. A child with either transient synovitis or early septic arthritis will respond to ibuprofen. Ibuprofen should not be used as a diagnostic tool, but as a treatment for transient synovitis once the diagnosis is made. The differential diagnosis includes Lyme disease, gonorrhea, post-streptococcal reactive arthritis and hemophilia. Aspiration of the hip with cell count, gram stain, and cultures is the definitive diagnostic procedure for septic arthritis.